Why Healthy Longevity Clinics Struggle to Sustainably Scale — A Systems Perspective
As healthy longevity moves from experimental science to real-world delivery, one question comes up repeatedly: why do so many clinics struggle to achieve sustainable scale and success?
There is no shortage of ambition. Across the world, hundreds of new clinics have emerged, backed by entrepreneurial clinicians, new-to-healthcare investors, or both. Many invest heavily in facilities, equipment and branding. Yet few manage to translate early promise into consistent clinical quality, operational resilience and long-term credibility.
In my experience, the limiting factor is rarely clinical intent. It is almost always systemic.
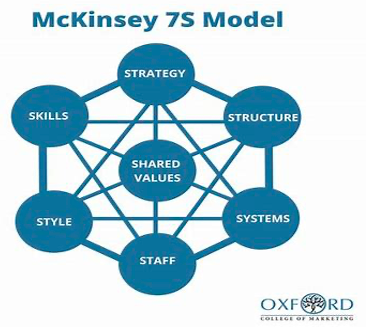
To make sense of this, I often return to a framework I first encountered long ago as a McKinsey management consultant: the 7S model. While originally developed for corporations, it remains a useful lens for understanding why complex endeavours succeed — or fail — when all the individual components appear to be in place.
The seven elements — Strategy, Systems, Staff, Structure, Style, Skills and Shared Values — are deeply interdependent. In healthy longevity clinics, misalignment between them is often what sabotages success.
Strategy
Many clinics struggle to articulate who they are truly for. Are they serving a narrow, high-end clientele or a broader population? Are they prioritising clinical depth or experiential differentiation? Are they purely to enhance clients’ physical wellbeing or to manage their health holistically? To detect and treat disease or refer clients to the official health system for these? Without strategic clarity, investment decisions — from facilities to staffing — can become random rather than reinforcing.
Skills
A good level of clinical excellence is essential, but skill mix matters. The balance between generalists, specialists, nurses, technicians and experts in advanced interventions - and the pathways between them - are rarely designed systematically. Too often, capability grows opportunistically rather than intentionally.
Structure
Healthy longevity clinics sit at the intersection of medicine and entrepreneurship. That tension plays out in governance. Questions around clinical autonomy, leadership oversight and multidisciplinary decision-making are often left unresolved, leading to friction rather than collaboration.The multi-disciplinary team can make a huge difference her.
Staff
Operational leadership is frequently underestimated. Titles, roles, incentives and routines shape behaviour more than mission statements. In clinics with high proportions of part-time staff, building teamwork, loyalty and continuity requires deliberate effort. Many staff recruited from conventional medicine can feel at sea in this new environment.
Systems
Digital infrastructure is one of the most common points of failure. Fragmented record systems, billing platforms and scheduling tools increase administrative burden for staff and dilute the client experience. Incentive systems, too, often reward individual performance at the expense of collective outcomes.
Style
Every clinic projects an unwritten narrative, whether intentionally or not. Are we essentially medical, luxurious, technological — or a confused mix? In a field that already struggles with credibility, mismatched signals erode trust quickly.
Shared values
These are perhaps the most elusive element, yet most important, as they are the glue that binds the organisation together. Clinics must constantly navigate tensions between client service, scientific rigour and commercial sustainability. Without explicit shared values, a ‘North Sea’ if you will, drift is inevitable — and difficult to correct once embedded.
I sometimes add an eighth ‘S’: Space. The physical environment is far from cosmetic. It shapes trust, perception of safety and professional seriousness, particularly in a field that still sits somewhat outside mainstream medicine.
Seen together, these factors suggest that successfully scaling healthy longevity is not primarily a clinical challenge. It is a systems challenge, requiring a high level of managerial professionalism.
As the field matures in 2026, success will depend less on isolated excellence and more on coherent design — clinics built as integrated systems rather than collections of well-intentioned parts. Those that recognise this early are likely to define the next phase of credible, scalable healthy longevity.
If you would like to talk about these issues I’d love to hear from you. [Chick here]